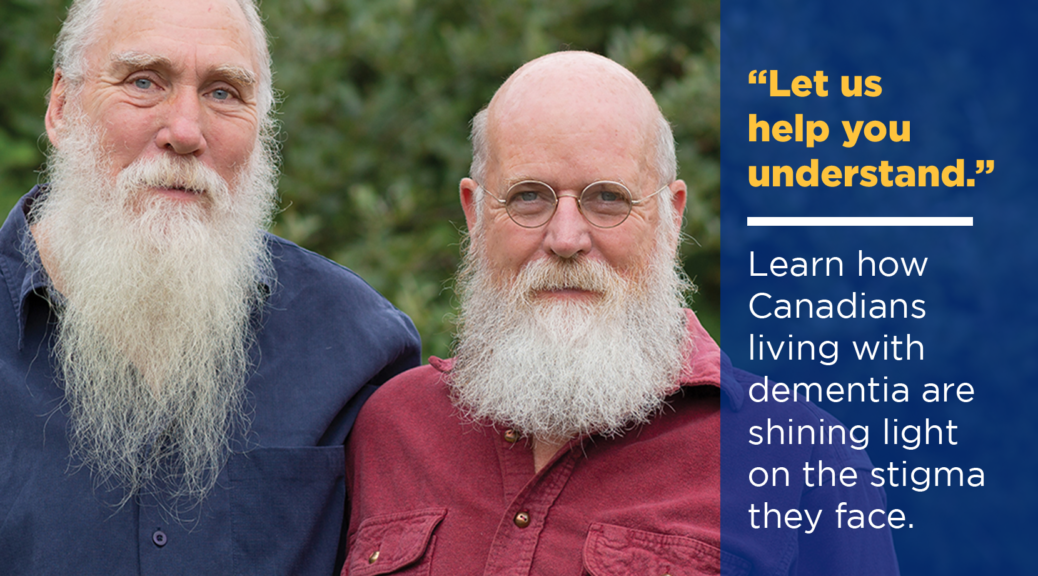
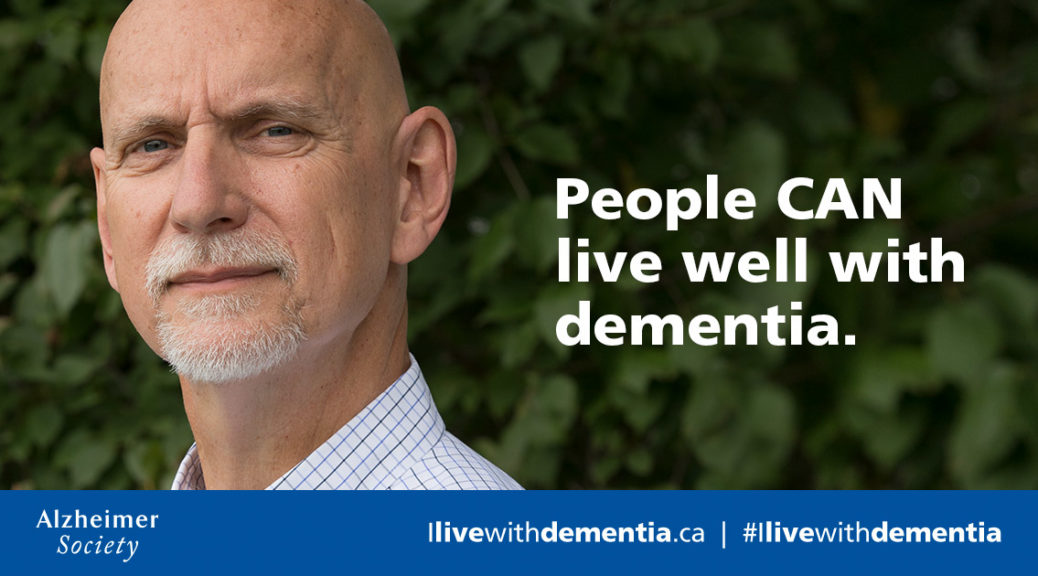
“Let us help you understand.” Learn how Canadians living with dementia are shining light on the stigma they face.
Everyone’s experience with dementia is unique – whether they are someone who has dementia, a caregiver or a family member of someone who is diagnosed. Each person has their own unique story to tell, even as they battle the stigma that faces them as someone living with dementia. With January being Alzheimer’s Awareness Month in Canada, the Alzheimer Society would like you to meet some of these people, and hear their stories. Read on to understand how Canadians living with…